Silos in Surgery: A Call for Cross-Team Connection
Incision · · 9 min readFrom diagnosis to discharge, surgical care involves several key teams. Although fundamentally interdependent, in practice, these teams tend to work in relative isolation from one another, providing what falls within their particular remit before responsibility passes along to the next.
In this blog, we look at how this both reflects and encourages the development of silos, and how these can impact the quality and efficiency of perioperative care. We share some strategies to help navigate breakdowns, optimize collaboration, and pool our collective strengths in order to hit the highest standards possible.

More Than a Business Buzzword
Silos, you may have heard, are now everywhere. Coming in at number 20 on the Forbes Glossary of Most Annoying Business Jargon, talk of “breaking down silos” has become a mainstay of boardrooms and workshops, striking fear into the heart of anyone hoping for a timely finish.
Part of the phrase's popularity surely comes from the commonality of what it describes. Many of us have seen problems caused by a lack of communication between different parts of an organization. Think surg techs not talking to sterile processing, anesthesiology not talking to recovery, surgeons not talking to anyone…
Over time, behaviors develop to support the aims of the team itself, rather than the organization as a whole. Inefficiencies build. Patterns repeat. Silos have formed.
In The Silo Effect, Gillian Tett (anthropologist, chair of the editorial board and US editor-at-large of the Financial Times) offers a broader take on these processes. According to Tett, silos within an organization represent a type of systemic fragmentation, creating a situation where “the right-hand doesn't talk to the left.” In light of the 2008 crash, she describes the structures of large investment banks, with internal desks forming a series of competing professional tribes, each with its own targets, lingo, incentives and identity. Seem familiar?

Outside a Cultural Bubble
As well as those within an organization, Tett describes the mental silos that individuals form based on their backgrounds and culture, creating a kind of extreme tunnel vision. People tend to see what they know. They surround themselves with affirming views and similar faces, propagating the same decisions and repeating the same types of mistakes. Food for thought...
Both kinds of silo — structural and individual — resonate strongly in the world of surgery. We organize our work according to what tasks fall under what teams, based on the traditional structures of hospitals and training programs. We form strong tribal identities and learned behaviors. We silo.
These processes, whilst imperfect, serve a very real purpose: they get the job done. “The modern world needs silos,” Tett explains, “[...] humans need to create some structure to handle this complexity.”
Talk of vaguely breaking down silos, then, sort of misses the point. It is the silo mentality — inward-looking, sharing-averse, resistant to change — that we should seek out. Stepping outside the bubble of our biases enables us to reflect on our processes, navigate our teams, and objectively improve our results. So, how can we do this in surgery? And how could this increase the quality of our care?

The challenge is not to rid ourselves of silos but to master them, instead of allowing them to master us.
— Gillian Tett, The Silo Effect
High-Risk Silos
Identifying silos in surgery is relatively straightforward, and most hospitals and care centers maintain a traditional, rigid organizational structure. (As a caveat, see Tett's chapter on the world of the Cleveland Clinic and pioneering CEO Toby Cosgrove.)
These structures can be seen in relation to the different stages of perioperative care, reflected in the timeline of a patient's surgical journey (Fig 1). Within each stage, several sub-stages form, based around the geography of where specific activities take place, and the specialized teams responsible for delivering them.

The intraoperative period (green in Fig 1) is of particular interest, not least because these are the processes that utilize the operating room (OR) and a large part of a hospital’s expenditure. In the OR, we see the coming together of a number of different teams and their workflows, creating a unique and safety-critical set of interactions. Often, several processes will run in parallel; one team is busy with one thing while another prepares the next.
We know, from quite an extensive body of research, that the complexity of these interactions creates a particularly high-risk environment — making it vulnerable to mistakes, information loss, and communication errors. These, of course, are some of the key products of a silo mentality.
Cross-Team Communication
Lack of communication between groups is perhaps the hallmark of a silo. Across fields such as aviation, nuclear power, and healthcare, communication failures are recognized and studied as a leading cause of adverse events, often with high-profile and heartbreaking consequences.
In the OR, researchers from the University of Toronto found communication failures in 30% of team exchanges, with one-third resulting in effects that jeopardized patient safety. In Washington, communication failures contributed to injury in 43% of perioperative anesthesia malpractice claims, with nearly half of these occurring in the intraoperative period. The majority of these failures were between an anesthesiology team member and a surgical team member — two of the primary silos of the OR.
As well as direct harm, OR silos create inefficiency. In Chicago, researchers conducted over 150 hours of direct observations and identified 67 communication failures in the OR. Of these, 36% were related to equipment, and 24% were related to not keeping team members informed of the progress of an operation. These frequently led to delays and inefficiencies.
In a wider analysis, a 2017 systematic review examined the application of a tool called process mapping to the intraoperative period. Across studies, they identified several common intraoperative points that introduced inefficiency; these often occurred at points where the workflows of one team interfaced with another, like patient transfer, instrument setup, and anesthetic handover.

Communication failures frequently occur when the siloed workflows of two or more teams fail to interface as planned
A Universal Surgical Language
So, what are some solutions to navigate our silos in surgery?
For this, we turn to another branch of silo study: data. Data silos represent data that belongs to one unit that this isolated from the rest of an organization. Although limiting access to data may seem logical, this practice has been shown often to propagate deeply unhealthy data — quickly breeding inconsistency and redundancy. Data silos tend to spiral exponentially, making it extremely difficult for anyone to get a clear picture of what’s going on.
In surgery, opening up data silos has consistently proven beneficial. Large-scale initiatives such as Integrated Care Pathways, Enhanced Recovery After Surgery, and the Perioperative Surgical Home have significantly improved surgical outcomes and efficiency through improved access to quality resources and country-level data. When teams share data and pool resources, it helps us to communicate and step outside of our traditional silos.
To this end, Incision has worked extensively with the concept of a universal surgical language. This methodology, built around a stepwise framework to standardize and communicate surgical procedures and concepts, has proven to reduce errors and improve performance. It is made accessible through an online academy containing over 750 courses, professionally filmed live in the OR. Incision Academy is accredited by the Royal College of Surgeons of England and has over 170,000 users across the world today.

Cross-Team Connectivity
On the work floor, facilitating information flow between teams is more challenging. It requires a connectedness that has been impossible until the widespread usage of mobile technology. All of this is now changing.
In a first-of-its-kind approach, Incision Assist is a mobile app that enables interdisciplinary teams access to their unit-specific, team-specific, and surgeon-specific resources and protocols. Assist is proven to improve information access, increase familiarity with equipment, and boost the efficiency of cross-team processes such as patient turnover.
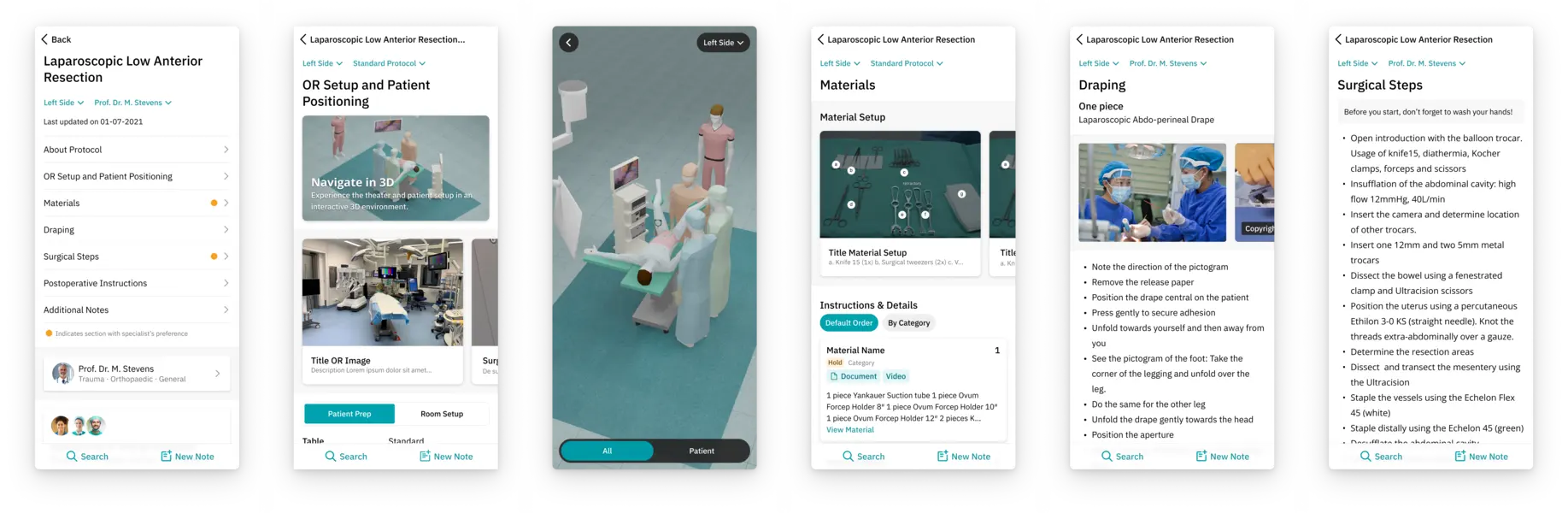
...In the holding bay, the pre-op team checks Assist. They look to see if everything is ready for anesthesia, including the video-guided system this anesthesiologist likes to use.
Meanwhile, the OR is prepped just the way this particular surgeon likes it. There is no confusion over equipment (this is all mapped out in a 3D OR in the app). The surgery starts on time.
Halfway through, recovery wants to check something about where the drains will be. Easy: just check the surgical steps in the app.
In recovery, the surgeon's post-op instructions are clear: no antibiotics, food after 4 hours, back to the ward, review tomorrow. The protocols are up-to-date, fully accessible, and all just a click or a scroll away — whatever tribe you work in...

By connecting our silos, rather than fixating on breaking them down, technology is enabling us to harness the collective strength of our teams. Here at Incision, we’re dedicated to writing blogs that inspire conversation, bring teams closer together, and educate in a dynamic way. When we learn together, we grow together, so join the conversation!







