4 Reasons Why Surgical Outcomes Vary
Ritsaart van Montfrans · · 8 min readThe chance that you require surgery at some point in your life is quite high (on average, people receive surgery about 9 times). Intense moments in the lives of patients, and an activity that receives enormous attention and dedication from teams in clinics around the world. At Incision, it is our mission to enable continuous surgical improvement that leads to better outcomes for everyone. The outcome of the operation, however, will depend on the clinic (and it’s surgeon & team) where you receive it. And variations can be quite large. Why is that? And why is it so difficult to improve?
Variation in outcomes
One of my first questions when starting to work in the area of surgery was: ‘how different are the outcomes of surgery between hospitals and countries’? In a world where many things are measured, it would seem to make sense that this information is available. However, it’s not always easy to find.
Some clinics openly publish outcomes of surgeries. But many also choose not to do so, often for logical reasons. The case mix between clinics can be quite different. And statistical relevance can be hard to achieve with sometimes only limited numbers of cases per clinic.
Where the numbers are available the variations can be substantial. A well-known example is Martini Klinik, the prostatectomy clinic in Hamburg. With an enormous case load (>2,500 per year) they have specialised to achieve very low complication rates. Incontinence 1 year after operation a few years ago was at 6,5% for Martini, whereas all clinics in Germany combined were at 43,3%. And 1 year severe erectile dysfunction was 34,7% for Martini vs 75,5% for Germany. As a 40+ male this is quite a difference for me...
ICHOM (International Consortium for Health Outcome Measurement) also provides data points, indicating 2x-5x (and upwards) differences between top and bottom 10% of clinics for operations in various countries. And there is more data, from national audits, from patient associations, from research, etcetera.
So, what is driving these differences?
With such dedicated surgeons and OR teams, how can it be that these differences exist? The mix of patients is of course always an issue, but the impact of that mix should become clear when the numbers get larger. I spent some time looking into this and the most important drivers appear to be the following:
1. What procedure is executed?
It’s a complex and dynamic profession. There are various ways to perform an operation. And within that many different variations can be used, with smaller and larger differences (e.g., in a colon procedure the ‘re-connection’ anastomosis can be done inside or outside the abdomen). Surgeons all have their individual preferences. And, new techniques, new devices and new data keeps adding new ways to operate. These new executions need to be tested, validated and disseminated around the world, which takes time.
2. Skills level of the surgeon
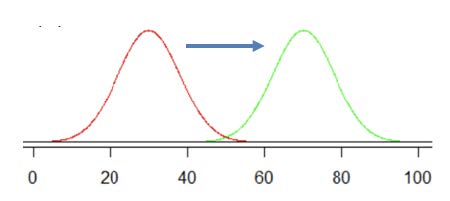
How good is the surgeon at executing the procedure? There is lots of evidence that experience levels of surgeons is very important. For example, Dr Jurriaan Tuynman showed recently that a new rectal cancer treatment lead to 12,8% recurrence for the first 10 cases, dropping to 5,4% for 10-40 cases and to 3,6% for 40+ cases. And many other studies show similar results. A strong case therefore for specialisation of surgical teams in certain types of procedures. Similarly, young surgeons and residents go through a learning curve, and there is an increasing awareness that trainings should be optimised to ensure the shortest possible learning curves.
3. Skills level and teamwork of the OR team
It’s not only the surgeon him/herself. Surgery is team work, with scrub nurses, anaesthetists, nurse anaesthetists and other assistants working together very closely. And, their level of skills and expertise, as well as the way they cooperate as a team, is therefore important. Training and skills levels seem to vary a lot between OR teams. Most training is done ‘in-service’, and the combination of hectic OR schedules and limited budgets results in very limited training moments. As a result, OR teams may not be fully trained or certified to use specific OR equipment. For example, in a survey we ran ourselves, close to half of OR team members in Netherlands rated there training level as insufficient (scoring less then a 6 out of 10). Cooperation within teams is often hampered by a lack of specific (workflow) tools, as common in other industries. One of my favourite writers on surgery, Dr. Atul Gawande, makes a great comparison in his ‘Checklist Manifesto’, showing how poor process support is for surgical teams, even though the complexity and importance would require it. And there are the ‘human factors’ in execution of surgery. They are present in 75% of aviation accidents, and they are known to be important in surgery as well. Malcolm Gladwell in ‘Outliers’ describes the levels of communication and how they attributed to airline crashes, for example Korean Airline flights in the 90s. When you see something going wrong in the OR, do you whisper a suggestion to the surgeon, or do you make a bold statement? Crew Resource Management (CRM) has been used a lot to improve this in airplanes, but the introduction of CRM in ORs is only limited. The video on ‘Just A Routine Operation’ is a telling example.
4. Access to resources
And lastly, of course there are differences in access to resources. In high-income settings, the latest devices can be found, such as robots and hybrid-OR’s. But in many mid-income and low-income countries devices, disposables etcetera are not available, impacting the possible procedures that can be executed.
Improving is challenging
So, the solution would seem to be easy. As a surgeon and team, just make sure you use the best method, train yourself and your team, make sure you collaborate well, and have all the equipment you need. Alas, matters are a bit more complicated. It’s not always easy to improve on these drivers for a number of reasons:
A. Lack of standards
For the vast majority of surgical procedures, there is no agreement (yet) on the best way to operate. There is no standard way to compare execution and compare outcomes. Research is the key instrument that is being used, but it focuses often on selected areas and investigates individual or limited research items. A reliable, acceptable and holistic way to exchange data is missing.
B. Speed of dissemination and implementation
Speed of dissemination of knowledge and new insights is hampered by the old-fashioned education for surgeons and teams. So, it can take many years for a superior surgical technique to be implemented around the world. And, the use of technology for communication and work support in OR teams is lagging other industries substantially, so that doesn’t help either.
C. Lack of staff
Around the world there are shortages of surgical staff, ranging from residents to scrub nurses. The growth of healthcare, inefficient education, and budget pressures are not helping to solve that point anytime soon.
D. Cultural challenges
As with the airline industry, the cultural factor in this is large. Healthcare is often reported to be a very hierarchical work environment, with differences by country. CRM aims to ‘foster a climate where authority may be respectfully questioned’, but daily practice in the OR shows how difficult this can be to achieve. Doctors are trained to achieve autonomy to treat cases, but with increasing specialisation there is an increasing need to move towards ’team autonomy’.

Incision’s approach
At Incision we try to make a contribution to this challenging topic. We focus on establishing a number of standards that help a structured approach. We apply all the tech solutions available now that can help (3D, AI, VR, CGI, etcetera). We are working to connect surgical professionals to better share knowledge, skills and data. And we create education and workflow solutions to help them.
So, lot’s of work ahead for us. In upcoming blog posts I will go into detail on a number of these, starting with the methodology we are using for standardisation.
In the mean time, please reach out to us if you would like to contribute to our work by sharing ideas or contributing to our projects. Please send me a DM, I look forward to hearing from you!
Curious what Incision's surgical e-learning platform can do for your hospital?
The Incision Academy contains over 500 high-quality video courses on surgical procedures to prepare for your work. Explore surgical procedures step by step in 2D & 3D, master basic principles and skills, anatomy, medical technology, and much more. We bring together everything that’s required to optimize OR performance.







