API for the OR, in 5 steps
Ritsaart van Montfrans · · 7 min readFrom a ‘Blackbox’ to ‘Best practice sharing’
The vast majority of surgeries is not standardised. For some procedures, guidelines or protocols are available. But mostly it’s up to the surgeon and its team to apply their own execution. Similarly, surgical reporting and outcomes of surgery are also not recorded in a standardised way across the world. Why is this relevant? As per my previous blog post, outcomes of surgery vary widely between clinics and countries. Part of the solution for this is to improve knowledge exchange and learn from best practices. But, how can you have a learning system if the exchange of data is so difficult? For any learning system to become better you must be able to understand what is being done, what the outcomes are, and how you can improve together. Parallels from other industries are abound. SMS took off when international technical standards were established. Airlines measure tire profiles in the exact same way across the world. Computer systems have API’s, a way to connect systems and extract data based on an agreed interface for communication. Healthcare is being digitised at a rapid pace. Standards are emerging for anatomy, for diseases (ICD codes), for cancer description (TNM staging), for clinical reporting (SNOMED codes), etcetera. Processes are increasingly supported with standard interfaces, such as those used in some countries in referrals by GPs to hospitals.
Surgery is lagging behind
Surgery, however, is not described in a standardised way. The same instrument may have different names, even within the same hospital. Procedural steps are described in many different ways, if at all. Outcomes are measured in a detailed way in research, but between countries and hospitals the parameters that are used to report the outcomes are different. Some pockets of standardisation are emerging. Take for example national audits, such as the colorectal surgery audits. Over the last 10+ years, standard outcome measures have been implemented, improved and measured. And as a result of this process, the outcomes of colorectal surgery have drastically improved. But once you cross the country border, other parameters are used and the comparison becomes difficult.
An API for the OR
What if we could describe the actions of a surgical team anywhere in the world in the same way? And describe their results in the same way, with clear definitions of the measurements? What if we can make a standardised ‘picture’ of how they work, and provide a ‘mirror’ for surgeons and their teams to make an insightful comparison with other teams? At Incision we are using a methodology that aims to achieve this in the years to come. I would like to share the elements of the methodology with you. And, most importantly, invite you to participate in this development with us.
1. How do you describe a surgery?
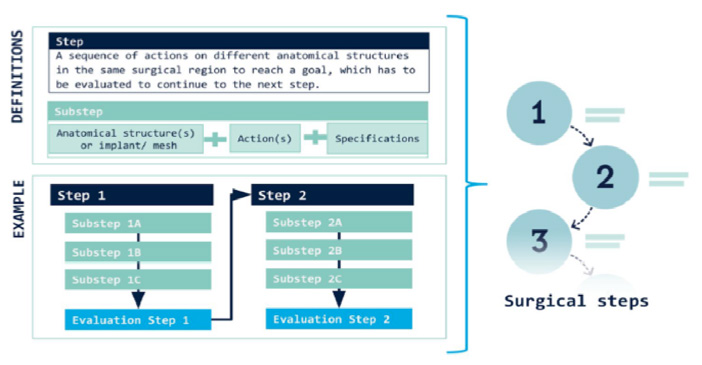
First step in the methodology is the description of the steps of a procedure. In our step-by-step methodology we use steps that are defined as follows. Every step in the surgery has a separate goal, which has to be achieved before continuing to the next step. Each step is divided in substeps; in which every substep describes an action on an anatomical structure or implant (see also our BJS Open publication on this, by Dr. T. Nazari). Next is the use of ‘words’. For all surgical actions we have defined the verbs to use, such as ‘incise’, ‘lift’, etcetera. With this step-by-step methodology we then describe a ‘Base’ version of a surgical procedure. As there is no standard for procedures, we use international guidelines where available and describe a commonly used execution (guidelines are often not very specific, and leave plenty of room for interpretation). In short, we believe that the best approach is to start with a ‘Base’ description of a procedure, and then take it from there to describe various executions.
2. How do you describe different executions of surgery?
Now, how to describe the variations to the Base Procedure? Together with surgeons from European surgical societies we have developed the methodology for this. The steps of the Base Procedure can be executed differently, based on a ‘Local Variation’. In the SurgMap project we are making an overview of these Local Variations per procedure, and typically we identify 8-15 of these variations per procedure. In addition, the execution of a procedure varies depending on the situation at hand. We have divided this into the following categories of Situational Variations: (i) Patient Characteristics (e.g., an obese patient), (ii) Disease caused (e.g., a large tumor) and Anatomical (e.g., a malrotation of the bowel). In the SurgMap project we map which Situations are important per procedure and how the surgical team acts differently (per procedural step) in these cases. Finally, most common Complications are identified and actions are described. It sounds a bit complex, but after having done the first 20-25 procedures it turns out that the methodology can be applied quite efficiently, and is able to capture the differences in surgical execution around the world.

3. How do you describe the actions of the whole team?
The first two steps are mostly about the actions of the surgeons. This third step is about the rest of the surgical team. Using a number of categories (OR devices, Patient position, Draping, Disposables, etc) the methodology describes the pre-operative preparations that the surgical team does. In addition, the team actions per step of the procedure are described. So, what is normally recorded in the OR protocol is now described in more detail, and in a more structured manner.
4. How do you describe the case-by-case execution of surgery?
In steps 1/2/3 the ’default’ execution of the surgical procedure is described. This is how a surgeon and his/her team normally work. However, specific patient cases are often different. The methodology aims to use the ‘default’ execution of the procedure as the starting point for a structured ’synoptic report’ per case, using exception-based reporting to indicate exceptions from the default execution. A first version of a synoptic report has been developed for Colorectal procedures together with an international group of surgeons, and we will be starting soon to gather additional inputs on this.
5. How do you describe the outcomes?
And finally, there is the description of outcomes. In order to create a ‘learning’ loop the relevance of surgical execution needs to be measured. Both in terms of clinical outcomes and efficiency/costs. Here, we will be connecting to outcome measurements as they are used in research, in audits and in initiatives such as ICHOM. We have started the first work, watch this space for progress!.
Conclusion: challenges ahead
It’s an exciting project to work on, but there are of course a few obstacles to be overcome. To do the exercise above takes a lot of time and dedication, and requires the help of many professionals around the world. Language is also a big topic. In the ORs around the world the local language is used, and for safety reasons this makes a lot of sense. Especially since the education level of the OR team does not always include english as a primary language. So, this adds a complicating layer to the project, and the need to establish the ‘words’ again for each new language. A big effort therefore, which will keep us busy for some time to come :). But, I like the phrase ‘restless patience’; it is a big task ahead but that doesn’t mean that we should not be starting it today in order to achieve a big impact later in time. More blogs on our approach to follow. In the mean time, please reach out to us if you would like to contribute to our work by sharing ideas or contributing to our projects.
Curious what Incision's surgical e-learning platform can do for your hospital?
The Incision Academy contains over 500 high-quality video courses on surgical procedures to prepare for your work. Explore surgical procedures step by step in 2D & 3D, master basic principles and skills, anatomy, medical technology, and much more. We bring together everything that’s required to optimize OR performance.







