Digital Guide to the Operating Room
Incision · · 13 min readWhen a surgical procedure is required the patient's care will be initiated by the operating room (OR) staff or surgical team. The responsibility of the operating room staff is to provide care and assistance to the patient within the duration of the procedure. The operating room personnel shares responsibility for the well-being and comfortability of the patient. Everyone within the surgical team possesses a unique staff role in the OR. The privacy and safety of all patients is the top priority for everyone.
This article will look into the design and layout of Operating rooms and what Operating rooms are all about using the Incision Academy courses Operating Room Introduction and Operating Room Design and Layout as the basis.
What Is the Operating Room?
The Operating Room, or OR, is a large, sterile room where surgeons operate on patients. It is equipped with surgical tables, monitors, and other equipment necessary for surgery. There are many types of operating rooms depending on the type of surgery. The room is typically cool and quiet, and the air is sterile and clean.
What does the inside of an operating room look like?
The typical operating room will consist of a surgical table that can be rotated and adjusted through the procedure. All tables have weight restrictions and removable pieces for the back and legs. This allows for more flexibility for the patient and optimal ergonomics for the surgeon and the team.
The operating complex has several rooms for changing, supplies and equipment. Most of the operating rooms have a separate room for scrubbing and preparing the sterile tables. Most operating rooms have a sluice that connects the operating room to the corridors of the OR complex to optimize the airflow in order to support infection prevention.

Next, there are the mounted lights and booms that are used to provide lighting during the procedure. These are adjustable and can be moved around to specific locations during the surgical procedure. Mounting the lights provide additional space for operating room staff and additional equipment that may be needed. Back tables are also used during every procedure. These tables are covered in sterile blue cloth and are used to hold the surgical instruments needed for the procedure.
All operating rooms consist of an anesthesia cart, oxygen, wall suction, and additional anesthetic gases. The OR contains additional space and tables for other surgical supplies and emergency equipment that may be needed at any given time. The operating room has several other rooms for hand washing, changing, supplies and equipment. For a surgical procedure to be successful, everything is carefully coordinated among the operating room staff from start to finish.
Operating Room staff roles
Everyone of the surgical team holds a crucial staff role during the procedure. The operating team members usually consist of sterile and unsterile divisions. The surgeon, assistants to the surgeon, and the scrub team are a part of the sterile division. As a part of the sterile division, you are required to perform surgical handwashing and wear sterile gloves, gowns, and masks. You are only authorized to handle sterile equipment and must remain in the sterile field area of the OR. The nurse anesthetist, anesthesiologist, circulating nurse, radiology technicians, medical device representative, and additional staff are a part of the non-sterile division. The operating room staff roles are coordinated amongst each other during the patient's surgery.
Typical operating room staff roles in the US are:
- Operating Surgeon
- Surgical Assistant
- Surgical Nurse (RN)
- Surgical Technologist
- Physician Assistant (PA, PA-C, APA-C)
- Nurse Practitioner (NP)
- Anesthesiologist
- Nurse Anesthetist (CRNA)
- Radiology Technician (Rad Tech)
- Medical Device Representative (MR)
The Operating Room Environment
The Operating Room Environment is a controlled and sterile environment where surgical procedures are performed. Surgeons and surgical assistants wear gloves, masks, and gowns in order to minimize the risk for infection. The patient is usually given an intravenous line to provide fluids and medication during the operation.

The operating room is also a place of many high-tech machines and equipment. Equipment like laparoscopic equipment, diathermy equipment, operation table, and suction may be found in most operating rooms.
Operating room design and layout
Here is a brief overview of the Operating room design and layout:
- The surgical table is placed centrally in the room, giving the surgical team easy access to the patient on the surgical table.
- A ventilation panel located directly above the surgical table is typically used to provide ventilation. By doing so, ambient air is directed away from the surgical site, carrying potentially contaminant dust particles with it.
- The anesthesia machine is placed at the end of the table where the patient's head is positioned and close to the OR door providing quick access for the anesthetic team in case of an emergency and anesthetic care that is convenient and efficient.
- The suction device can be used to evacuate blood, body fluids, and smoke during surgery. This makes the suction device a necessary component of surgical procedures and anesthetic care provision.
- A refrigerator is used to preserve specimens and store medications at desired temperatures.
- At least one operating light is installed directly above the surgical table. The lamp head can be adjusted to focus the light at different angles and intensities.
- The warming cabinet should be warmed to prevent hypothermia (leading to coagulation disorders).
- The position of the surgical team depends on the specific procedure to be carried out.
- The temperature of the Operating room is usually cold. The patient is kept warm using warmed blankets and/or mattress. Working under an operating light with protective gears on might cause the team to sweat, which can, in turn, compromise sterility.
Infection Prevention in the Operating Room
Infection Prevention in the Operating Room is of the utmost importance. Operating rooms are a breeding ground for bacteria and viruses, so it is essential to take precautions to prevent infection spread.
One of the advantages of cool temperature in the Operating room is microorganisms grow slower when subjected to lower temperatures. One of the most important things you can do is to ensure that all your surgical equipment are clean and sterile. You should also make sure that your hands are clean and that you are wearing a sterile gown and gloves.

Operating room zones
The Operating Room is divided into different zones (sterile, clean, protective, and disposal) to prevent air contamination and regulate materials' transportation.
The sterile zone
The sterile zone consists of the Operating rooms and clean preparation areas. In this zone, the highest level of aseptic conditions needs to be maintained. The ventilation system helps maintain air pressure gradient, minimizing airflow from the corridor to the OR.
The clean zone
The clean zone consists of the store areas, preoperative/holding room, recovery room, or PACU and OR staff rooms. It surrounds the sterile area and connects it to the protective area. Only staff wearing appropriate surgical wear should enter the clean area.
The protective zone
The protective zone includes dressing rooms, reception, and waiting areas. The zone surrounds the clean zone and forms a protective area between the clean zone of the OR and the rest of the hospital.
The disposal zone
The disposal zone includes the decontamination rooms and disposal corridors. The soiled instrument uses linen. Operating debris is removed via the disposal zone.
Basic operating room instruments
Basic operating room instruments are the basic tools that are used in surgery. These include:
- Needles
- Blades
- Gauzes
- Diathermy
- Retractors
- Scalpel holders
- Scissors
- Forceps
- Clamps
- Needle drivers
- Large Clamps
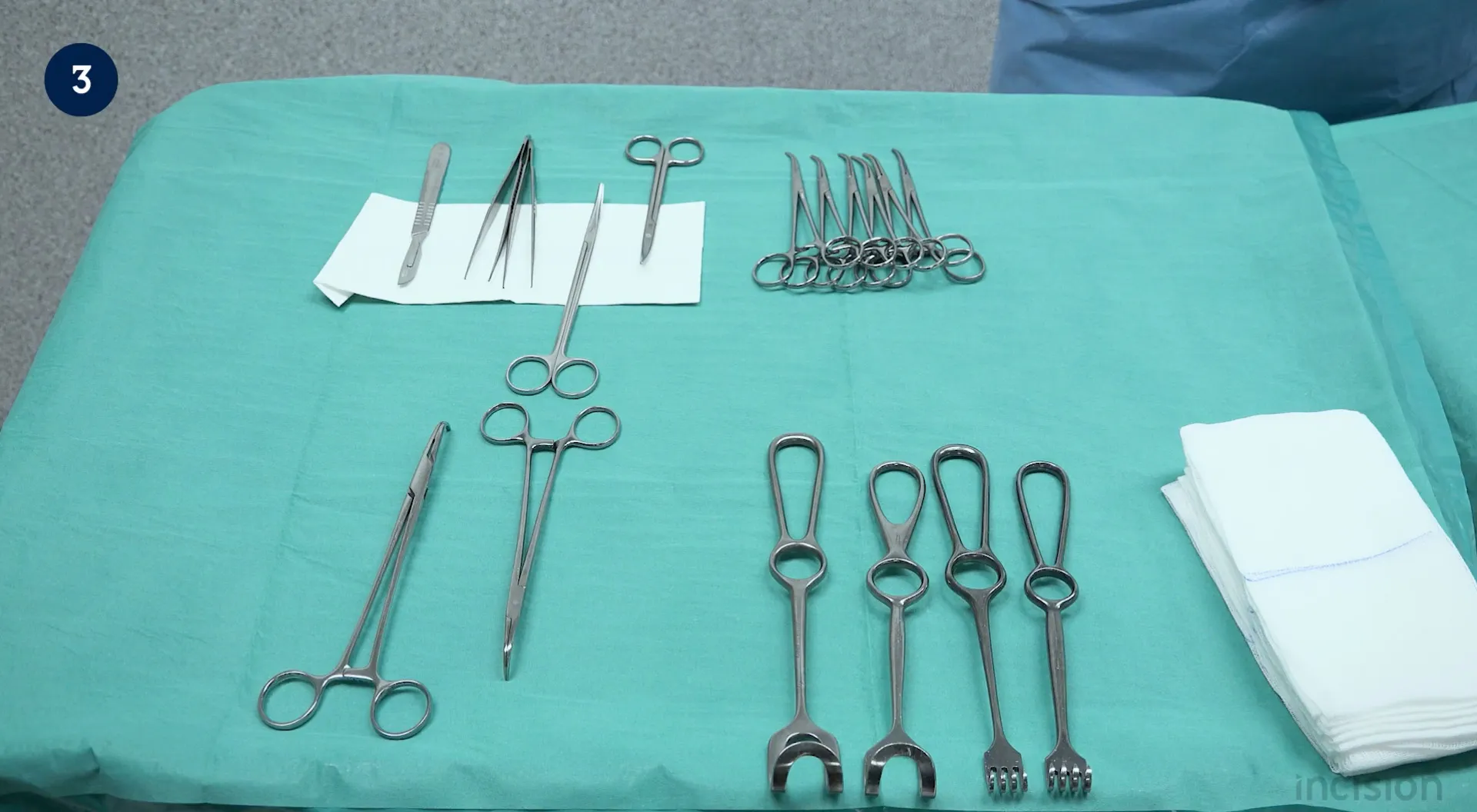
Handling basic operating room instruments
Careful handling of instruments is essential in the Operating room, The following tips regarding the handling of basic instruments can be very helpful:
- A needle can be placed in a needle holder in different ways based on the desired stitching. Usually, the needle is perpendicularly held near its midpoint in the tip of the jaws.
- The blade is placed with a clamp or needle driver on a scalpel holder. The blade can be removed with a blade remover or forceps. Multiple grips are possible according to the desired type of incision.
- When handling forceps, more force can be applied by holding it at its tip.
- To open a clamp, the cremaillere is released without simultaneously opening the clamp. The legs of the clamp are pushed towards each other and then away from each other before the clamp is opened.
After these instruments are used, they are cleaned and disinfected. The cleanliness and functioning of instruments are confirmed by sterilization department personnel. Packaging of surgical instruments and devices is done with the consideration of sterilant reaching its content and maintaining sterility until needed. Sterilization can be done with steam (an autoclave) or chemicals.
Learn more about basic operating room instruments and handling on this page which includes video content with tips and tricks.
Patient positioning
In the operating room, it's essential that members of the surgical team are able to safely position the patient on the surgical table in a number of different positions. An operation sheet is spread out on the already prepared operation table. It has an underlay that can tuck in the arms and transfer the patient to the hospital bed. The patient bed is placed parallel to the operation table in the OR. The rails are lowered, and the bed is placed next to the operation table to transfer the patient, then placed on brakes. The transfer board is moved, and the patient moves to the middle of the table. The arm board is installed, and the patient places their arms over the arm boards.
Gloving and dressing by yourself
Keep your arm in the gown's sleeves till you put on your gloves. The circulating nurse will help tie the strings attached to the neck and waist. Pick up the right glove with the left hand and allow the hand and fingers to maneuver themselves into the glove. Pick up the left glove with a sterile right hand and repeat the process. Stand in front of the circulating nurse and turn around to allow her to close the gown.
Patient skin antisepsis and draping
To avoid surgical site infections, the skin is cleaned and disinfected around the incision site. The agents used for this purpose should be applied rapidly, have a fast onset of action and a long duration of action. The alcohol-based agents are more effective than the aqueous ones, though aqueous agents are preferred if the patient’s skin is sensitive to alcohol.
Skin disinfection
Disinfection of the patient's skin can be done with chlorhexidine or povidone. Visible areas like the face and neck can be scrubbed with uncolored chlorhexidine. The newly applied chlorhexidine should not be touched. Perineal and the mucosal regions are preferably cleaned with povidone.
Draping
After the disinfectant has completely dried up, the small rectangle drapes are placed on the sides. A large drape is placed on the caudal side over the feet. The middle is determined, and the drape is pasted towards the lateral side. Another large drape is placed on the cranial side towards the anesthesiologist to separate the anesthesiologist from the surgical area. The middle is determined, and the drape is pasted from the middle towards the lateral side.
Operating room hazards
Operating room hazards can include everything from surgical tools that can cause injury to personnel to the potential for infections.

Sharp objects
Many sharp objects in an operating room can cause injury if not handled properly. These objects include scalpels, scissors, and needles. Without proper precautions, these sharp objects can result in a serious injury to the patient or medical personnel. Surgical tools, like scalpels, needles, and scissors, should be handled with care by healthcare providers. All sharp objects should be properly sterilized before being placed back into the operating room.
Infections
Using contaminated instruments during surgery can cause an infection to spread through the patient's body. These infections are often life-threatening and require immediate attention. To prevent the spread of infection, healthcare providers should only use sterile instruments. Additionally, all instruments that come in contact with the patient's body should be properly disinfected.
Strains
When a patient is malpositioned on the operating table, this can easily result in muscle strain or compromised nerves. A strained muscle can be incredibly painful, especially when the injured part remains inside the body. If a patient is undergoing surgery and complains of pain, this might be caused by malpositioning on the operating table.
Fire
Although rare in modern ORs, a fire outbreak can still occur. ORs are designed considering the correct location of fire extinguishers, installation of fire alarms, and gas shut-off valves.
Inadequate ventilation
If the air quality within the operating room becomes too poor, it can become toxic and dangerous for patients.
Leaving the operating room
Firstly, all sharp items are removed and placed in a separate container, then the drapes are removed and the patient covered up. The arm boards and other attachments to the bed are also removed. The hospital bed is placed parallel to the operating table and put on brakes with a roller board on it. The sheet is pulled over the patient, allowing the patient to roll over to place the roller board underneath the patient. The person standing at the head counts, and on three, everyone transfers the patient. After the patient is transferred, the roller board is removed, and the patient is covered with the bedsheet. The bed rails are lifted, and the patient can leave the OR. Afterwards, a number of steps are performed by the surgical team in post operative care.
Conclusion
Whether at the beginning of your career or towards the end, you should always be one step ahead. Knowing the ins and outs of an operating room is crucial to performing well and ensuring no mistakes are made. To ensure success within the operating room, know its hazards and how to avoid them.
About the author

Incision Nurse(s) are scrub nurses and nurse anesthetists creating courses for the Academy. The content we create is always checked by perioperative team members from client hospitals. By understanding their needs, we design what we believe to be the best solution to help healthcare professionals perform their daily tasks. The videos are intended to provide quick and concise overviews of the skills and concepts, relevant to the practice of scrub nurses and nurse anesthetists.







